COVID-19 and autoimmune rheumatic diseases: Vaccine insufficient protection against Omicron


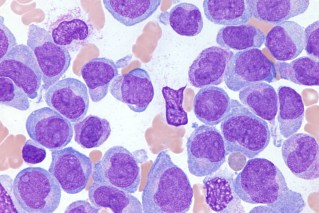
Autoimmune rheumatic diseases attack the joints, muscles, bones, and organs. Photo: Getty
A new study has found that mRNA vaccines (those from Moderna and Pfizer) don’t create enough antibodies to protect against the Omicron variant in people with autoimmune rheumatic diseases.
Autoimmune rheumatic diseases (ARDs), including rheumatoid arthritis, lupus and scleroderma are debilitating, painful conditions that cause the immune system to attack the joints, muscles, bones, and organs.
Korean researchers described the vaccine-induced immune response in these patients as “exceptionally weak” against Omicron (now the prevailing strain the pandemic) and highlights ‘‘their vulnerability to breakthrough infections’’.
A breakthrough infection is an infection with a virus after you have been vaccinated against it.
A complex situation
From the beginning of the pandemic there were concerns that people with these conditions were in for a particularly rough trot.
Subsequent research found they have a slightly higher risk of infection and a greater risk of serious illness.
Vaccine-induced protection was sub-optimal and complicated because of the immunomodulating medications that many patients take routinely.
One study found that patients on most immune-suppressing drugs had an 11 per cent reduced risk of needing invasive ventilation.
On the downside, according to a study in the Lancet, one medication, Rituximab, has become increasingly associated with worsening severity of COVID-19 illness and increased deaths.
Still, for ARD patients, dealing with COVID-19 is tricky.
A review published in February advised that people with immune or inflammatory rheumatic disease who experience mild COVID-19 symptoms should stop taking immunomodulating medications for one to three weeks from the onset of disease.
Those with poor outcomes should stop taking their immunomodulating medications and consider treatment with antiviral medications.
The new study
According to a report at Australian Doctor, the study was conducted in early 2022 during a surge in COVID-19 cases in South Korea, and involved 94 healthy healthcare workers and 149 people with ARDs.
Blood was collected from the participants at enrolment and about 15 weeks post-second dose or eight weeks post-third dose.
The team, led by doctors at Chung-Ang University College of Medicine in Seoul, examined the blood response to Omicron infection at 15 weeks after a second mRNA COVID-19 vaccine dose, or eight weeks after receiving a third mRNA booster.
People with ARDs exhibited lower response or protection after the second dose to Omicron (11.5 per cent) than the healthy healthcare workers (18.1 per cent).
After the third dose, a significant difference in response was observed – 26.8 per cent in people with ARDs versus 50.3 per cent in the healthy group.
The results of this study do not mean that the COVID-19 vaccine is no longer effective for people with ARDs.
As the February review makes plain: ‘‘People with immune or inflammatory rheumatic disease are strongly recommended to receive SARS-CoV-2 vaccination, including booster doses if recommended, despite some evidence of a diminished response in particular groups.’’
Bottom line: The study is a warning shot. As the virus changes, further research is needed to examine vaccine efficacy in people with autoimmune diseases.