Severe COVID-19 patients: Prescribing steroids cuts the death rate in half


All Australian jurisdictions except the NT experienced major levels of excess mortality in 2022. Photo: Getty
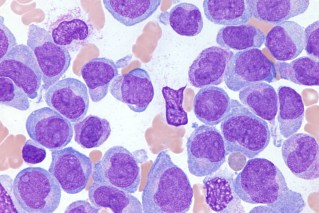
Over the past year, researchers from the University of Florida (UF) have published a series of studies that provide a clear and devastating prognosis for people who are hospitalised with severe COVID-19.
In July, they reported that people who had seemingly recovered from severe COVID-19 were likely to end up in hospital again with ongoing complications from the disease.
In December, they found that those who have recovered from severe COVID-19 are more than twice as likely to die in the following year than people who have not contracted the virus.
The pointy end of ‘long COVID’
These complications and deaths are further evidence for the mysterious condition now known as ‘long COVID’.
As we reported last week, despite widespread scepticism, ‘long COVID’ is a real thing.
The latest findings from UF give a refined understanding of who, among these patients, is most likely to die. And what can be done about it.
First, they found that the severity of a patient’s inflammation while in hospital might predict their risk of ongoing serious health problems, including death.
They concluded that severe inflammation during hospitalisation increases “the risk of death within one year from seeming recovery by 61 per cent”.
How to lower this risk
The researchers found that this risk of dying in the next year can be cut in half if patients are prescribed anti-inflammatory steroids when they’re discharged from the hospital.
These common steroids “lowered the increased risk of death linked to severe inflammation by 51 per cent”.
The authors argue that “prescription of steroids upon discharge from hospital for COVID-19 should become standard”.
These findings aren’t a great surprise.
In September 2020, the World Health Organisation changed its advice on hospital treatment and, as a Conversation piece reported, strongly recommended that corticosteroids be adopted as a first-line intervention for the sickest patients.
It’s important to note that people with mild cases of the disease should not take steroids, because they will likely interfere with and undermine your recovery.
COVID-19 as a chronic illness
First author of these studies is Professor Arch G Mainous III, vice chair for research in the Department of Community Health and Family Medicine at the University of Florida Gainesville.

Researchers say COVID-19 should be considered as a potentially chronic illness. Photo: Getty
He said there was a case for COVID-19 to be investigated as a potentially chronic illness.
“When someone has a cold or even pneumonia, we usually think of the illness being over once the patient recovers. This is different from a chronic disease, like congestive heart failure or diabetes, which continue to affect patients after an acute episode,” Dr Mainous said.
“We may similarly need to start thinking of COVID-19 as having ongoing effects in many parts of the body after patients have recovered from the initial episode.”
He said once the importance of ‘long COVID’ after seeming ‘recovery’ is properly recognised, “we need to focus on treatments to prevent later problems, such as strokes, brain dysfunction, and especially premature death”.
In these studies, Dr Mainous and colleagues investigated the electronic health records of 1207 adults hospitalised in 2020 or 2021 after testing positive for COVID-19 within the University of Florida health system, and who had been followed up for at least one year after discharge.