Pancreatic cancer good news: Two breakthrough studies in one week

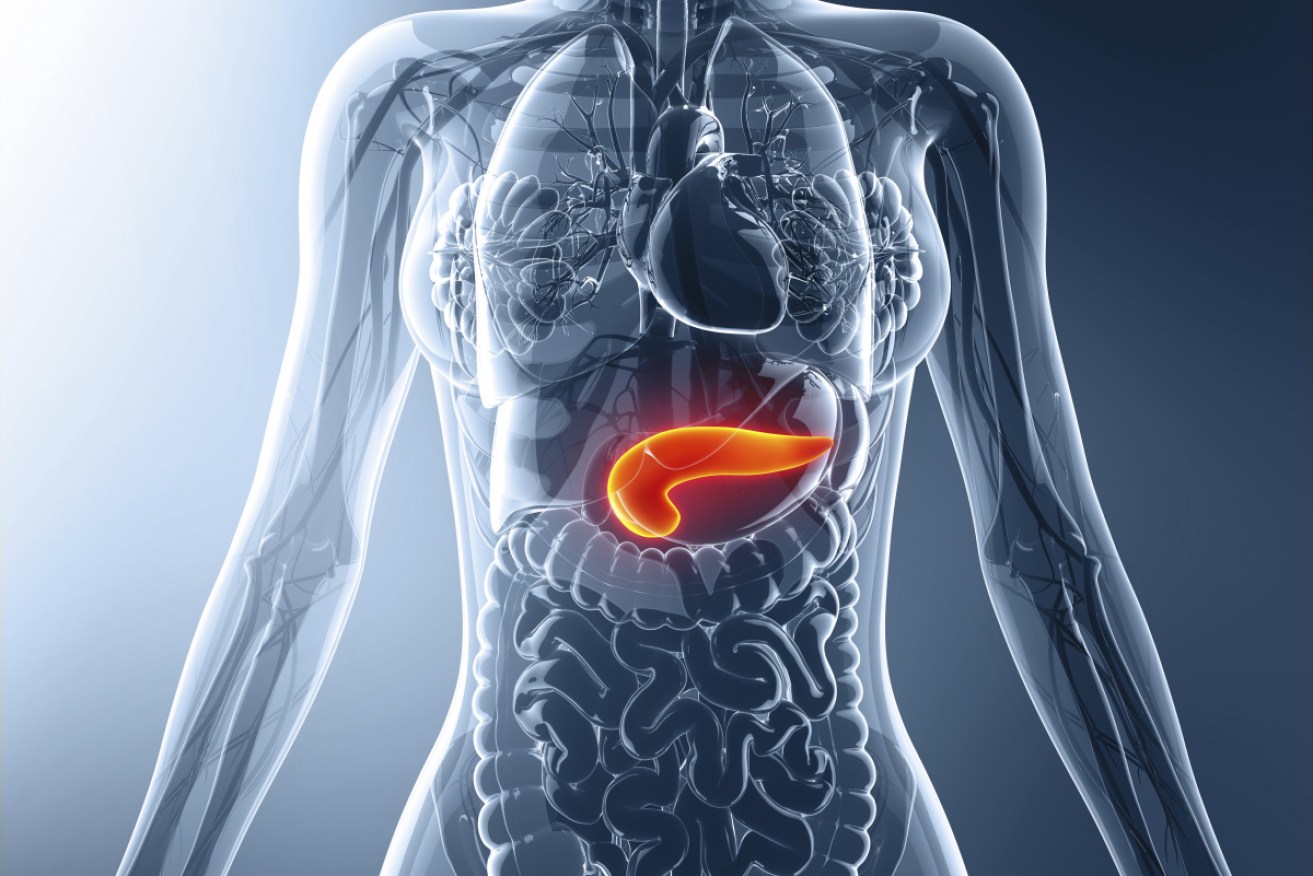
Two new studies bring a rare burst of optimism to the treatment of fast-spreading pancreatic cancer. Photo: Getty
Scientists from Sydney’s Garvan Institute of Medical Research have announced findings they hope could slow the spread of pancreatic cancer.
Researchers found that reducing the levels of a molecule called perlecan leads to a reduction in the spread of pancreatic cancer – and an improved response to chemotherapy, in an animal model.
The quick spreading of cancer from the pancreas is the main cause of pancreatic cancer-related death.
The early stage of pancreatic cancer generally has no symptoms; subsequent late diagnosis has an average survival rate of three-and-a-half months.
Moreover, chemotherapy tends not to be effective because pancreatic tumours are protected by a kind of hard shell.
Looking at the material that holds an organ in place
The researchers found some pancreatic tumours produce more perlecan than others to remodel the environment around them, which helps cancer cells spread more easily.
Perlecan also protects tumours against chemotherapy.
Led by Associate Professor Paul Timpson, head of the Invasion and Metastasis Laboratory, and Dr Thomas Cox, leader of the Matrix and Metastasis Group, the research could provide a viable path to more effective treatment options for pancreatic cancer and possibly breast and prostate cancers.
“Pancreatic cancer is very aggressive, and by the time most cases are diagnosed, the tumour is often inoperable,” said Associate Professor Timpson in a prepared statement.
New focus reduces spread, boost drug therapy
“What we’ve discovered in this study is a two-pronged approach for treating pancreatic cancer that we believe will improve the efficiency of chemotherapy and may help reduce tumour progression and spread.”
The focus of this research was to investigate why some pancreatic cancers spread, while others appear to stay in one place.
They took a lateral step in comparing the tissue around tumour cells in both metastatic (spreading) and non-metastatic (non-spreading) cancers.
This tissue is known as the matrix – and acts like a glue that holds different cells in an organ or in a tumour together.
(The video below shows how pancreatic cancer cells (green) spread along matrix fibres (purple) within the body.)
Using mouse models, the team extracted fibroblasts – cells that produce most of the matrix – from spreading and non-spreading pancreatic tumours.
Some cancer cells teach others to be more aggressive
They found that cancer cells from a non-spreading tumour began to spread when mixed with fibroblasts from a spreading tumour.
“Our results suggest that some pancreatic cancer cells can ‘educate’ the fibroblasts in and around the tumour. This lets the fibroblasts remodel the matrix and interact with other less-aggressive cancer cells in a way that supports the cancer cells’ ability to spread,” said first author Dr Claire Vennin.
“This means that in a growing tumour, even a small number of aggressive metastatic cells – a few bad apples – can help increase the spread of other, less aggressive cancer cells.”
Poo transplants choke tumours
Meanwhile, in another promising study published this week, University of Texas researchers found that “a key difference between the few pancreatic cancer patients who survive long term and the many whose disease overcomes all treatments is the bacterial signatures on their tumours that either stimulate or suppress immune response.”
The researchers showed that faecal microbiota transplants (FMT) from long-term human survivors prompted an immune response and stifled tumours in a mouse model of the disease by altering the bacteria on the tumour.
This is the latest and somewhat startling example of gut health playing a powerful part in treating challenging conditions.
In this instance, long-term pancreatic cancer survivors – a rare cohort – have a more diverse tumour microbiome than those who die quickly.
“Results of the FMT experiments represent a significant therapeutic opportunity to improve pancreatic cancer treatment by altering the tumour immune microenvironment,” said senior author Florencia McAllister, MD, assistant professor of Clinical Cancer Prevention at MD Anderson.
“There is promise here but we have a lot of work ahead.”