Too hot to handle: Women’s health still taboo in Australia

Systemic issues in healthcare delivery and medical research mean women often suffer poorer health outcomes. Photo: Getty
It was a Thursday evening in October. I found myself at a beautifully curated “intimate” women’s health event, facilitated by local businesswoman Rose Bonasera.
I’m certainly no prude when it comes to women’s health. Like many women who have been diagnosed with endometriosis in the past decade, I’ve been forced to take my health into my own hands. After a male GP told me to “have a baby, it will make it go away”, I lost all faith in the system.
I was expecting to pick up a titbit or two that evening but wasn’t prepared for the bomb that was about to be dropped on me – a masterclass in menopause. Safe to say, I still haven’t recovered.
What took me aback the most were two things; how significant a condition menopause is, and the fact that we lose more than 10 per cent of women from the workforce prematurely because of it.
How are we not up in arms about this statistic?
After comfort-eating too many canapés, I worked up the courage to speak to one of the panellists to find out more. An academic, she is hoping to get more funding to do her PhD research on menopause, but is finding money scarce. If only menopause affected men, I thought to myself. There would be millions of dollars thrown at it quicker than you can say Adelaide 500.
Significant impact
Menopause typically affects women aged between 45 and 55, an age when many men really hit their prime. In fact, the Workplace Gender Equality Agency found that while a greater proportion of men move into leadership positions as they age, the proportion of women who occupy leadership roles increases between 18 and 44 years and then significantly decreases.
Women become invisible as they age. While women are literally disappearing from the workforce due to menopause, women over 50 are also the fastest-growing cohort of homeless people, and First Nations women and those with disabilities are particularly vulnerable.
I digress.
You’ll have to forgive my ignorance on menopause, it was deliberate. The truth is I’ve always treated menopause as a future Anna problem. As a 37-year-old single woman, I have enough on my plate. I was asked the other day if I had thought about freezing my eggs. In the current cost-of-living crisis, my eggs and I will be cohabiting for the foreseeable future.
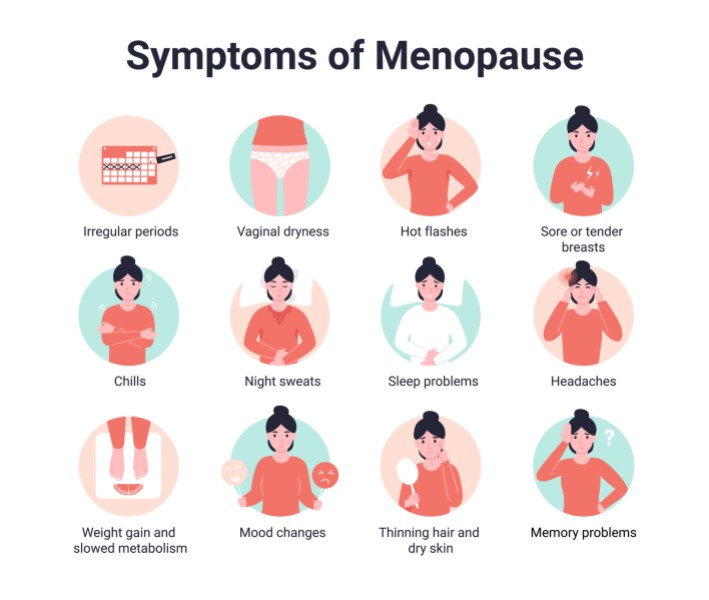
The symptoms of menopause are varied. Photo: Getty
‘Silent’ conditions
Speaking of invisible, have you noticed how women’s health issues like endometriosis and menopause are described as “invisible” diseases or “silent” conditions? I appreciate they are invisible in nature because they occur largely in areas we can’t see, but they remain silent conditions because we fail to speak about them as mainstream public health issues. Periods, infertility, miscarriage and menopause are still in many ways taboo.
There are glimmers of hope, with the announcement of a Senate inquiry into the issues related to menopause and perimenopause.
Perimenopause made national news when Imogen Crump experienced a perimenopausal hot flush live on television. Coincidentally, the economic impact of menopause is also starting to make headlines. In 2022, superannuation peak body, the Australian Institute of Superannuation Trustees, estimated menopause costs female workers more than $15.2 billion each year in lost earnings and superannuation.
It’s not just women who are paying the price. Macquarie Business School has crunched the numbers on the cost to Australian businesses. The estimated turnover cost to Australian organisations is more than $10 billion annually.
It’s important that we have these conversations, not just to overcome taboos and better support women in the workplace, but to encourage more investment in medical research and treatment so that women experience better health outcomes and we all benefit.
Substandard health care
Systemic issues in healthcare delivery and medical research mean women often suffer poorer health outcomes. A 2023 study of menopause treatment in Australia, by Davis and Magraith, featured in the Medical Journal of Australia, found that “lack of clinician knowledge, poor access to services, negative attitudes, and lagging research have led to substandard menopause‐related health care”.
While some symptoms of menopause are more well known, like hot flushes, fatigue, brain fog and mood changes, menopause also causes biological changes that may increase women’s risks of cardiovascular disease, diabetes, osteoporosis and some cancers.
The study noted that in light of these risks, “it should be expected that health-care providers, especially general practitioners, are equipped to provide evidence‐based menopause advice to the 3.28 million Australian women aged 40–59 years. Sadly, this is not the case”.
On average, it takes women seven years to go through perimenopause and menopause. Hardly a hot flash in the pan. More than 70 per cent of women are in the workforce at the time they transition through natural menopause. Yet despite these serious symptoms and chronic health risks, there remain significant research and knowledge gaps about the transition.

In the pursuit of gender equality, women’s health is key. Photo: Getty
Women I know experiencing menopause also face the double burden of responsibility of care for both their children and elderly parents. These women are not only making valuable contributions to the workforce but are also playing important (unpaid) roles in the lives of others. When we invest in women, we invest in the community.
The World Economic Forum has found investment in women is unrivalled in its return on the investment for the health of all society. Investing in women’s health is not just an investment in individual women but their families, their communities, and the economy.
High yield investment
It has found that a $300 million investment into research focused on women could yield a $13 billion economic return. However, a lack of action on women’s health has enabled social and economic backslides and has widened the gender gap globally. In the pursuit of gender equality, women’s health is key. Yet our leaders continually fail to prioritise it.
Women’s bodies are unique in that they are regulated and legislated in a way that men’s are not.
If some policymakers put the same attention and effort into promoting policies that address health inequities as they currently put into trying to control women’s bodies, we would be so much closer to gender equality.
So, what can we do to tackle taboos and get women’s health front and centre in Australia?
Framing expenditure on women’s health as an investment rather than a cost is a good start. The Women’s Equality Taskforce has put a dollar figure on what the Australian economy stands to gain from removing barriers to women’s full and economic participation – it’s a whopping $128 billion.
In addition to the turnover costs to businesses, they also lose the experience and expertise of women who leave the workforce. Macquarie Business School makes the important point that supporting menopausal women to remain at work will increase the number of women in leadership positions, contributing to greater gender equity in senior roles.
It was refreshing to hear the ‘M’ word pop up at a Fearless Female event I attended recently, with an incredibly impressive managing director willing to share her experience and struggles. However, there remains little research on menopause and work which limits the guidance that is available for employers. This is a gap that should be addressed.
Actions overseas
There are health initiatives rolling out overseas that may well show us the way.
The UK government this year made menopause treatment more accessible to women, by providing cheaper hormone replacement therapy for menopause through a new prescription prepayment certificate. The certificate will help around 400,000 women save hundreds of dollars a year, reducing their HRT costs to less than $38 (£20) a year. Making treatment more affordable and accessible for women is a good place to start.
An array of policy and public health reforms could be used to help ease the financial and physical burden on women. It’s why public conversations about women’s health are important. Greater awareness of endometriosis has seen increased funding for research and care. Similarly, interstate we have seen subsidies provided for IVF treatment. Could this be the start for menopause?
Giving women’s health the primacy it deserves on our public policy agenda is an important step towards gender equality. It’s time to remove the cloak of invisibility around women’s health.
Dr Anna Finizio is a former public policy and economics manager, a Liberal Party member and former ministerial adviser, and the SA Representative for the Hilma’s Network.